Hip labral tears can be a significantly debilitating hip condition. Without appropriate rehabilitation and treatment, this injury can lead to long-term issues such as worsening pain and dysfunction. It’s important to understand the what the condition is, the relevant management options and what they encompass. Here are some essential tips for managing tears of the hip labrum.
ANATOMY
Before discussing the management options, it’s important to understand the anatomy of the hip labrum. The hip labrum is a smooth U-shaped cartilage that sits inside the sockets of the pelvis (also known as acetabulum). Highlighted in yellow in the image below, it deepens the socket for the thigh bone (femur) to fit into the acetabulum. Consequently, this provides additional stability and protection to the hip joint. As the hip absorbs a lot of the body’s impact from activities such as running, a lot of rotational and compressive forces act on the hip labrum.
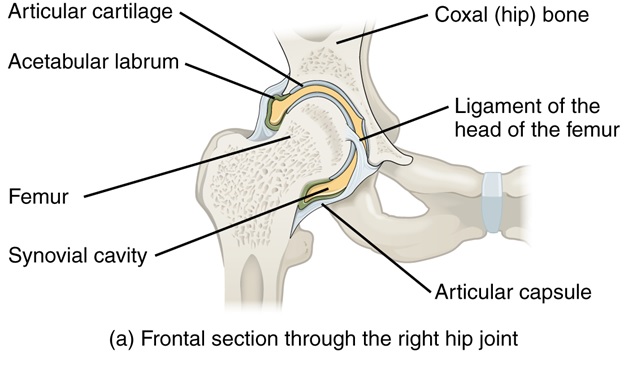
Image 1. Frontal view of the hip joint and labrum.Source: https://commons.wikimedia.org/wiki/File:916_Hip_Joint.jpg
Labral Injuries and Tears
Acetabular or hip labral tears are particularly common in athletes particularly in sports such as ballet and hockey. 2 common mechanisms cause labral tears include:
- Overuse injuries which may include structural changes within the hip joint (e.g. hip dysplasia, femoroacetabular impingement, etc.) and/or repetitive movements (e.g. pivoting, running)
- High impact trauma (e.g. motor vehicle accidents, falling, twisting)
Clinically, diagnosing labral tears are still difficult unless radiological imaging is conducted. However, symptoms that sufferers may face include:
- Locking and clicking
- The feeling of instability
- Groin and frontal hip pain especially when weight bearing
- Reduced hip strength and mobility
Diagnosis
As mentioned above, diagnosing a hip labral tear is very difficult unless investigative imaging (such as an MRI) is conducted. However, imaging should not be considered unless 6-12 weeks of physical therapy has been attempted. Reasons why imaging should be withheld initially include:
- Imaging is expensive and may not necessarily represent the underlying reason for the ongoing hip symptoms.
- Up to 42% of people without hip pain are ‘positive’ for labral tears on imaging. This shows the unreliability of these examinations.
- Even if imaging is positive for labral tears, rehabilitation is usually the first line of management. In many cases, athletes who have ‘labral tears’ also have significant hip weakness and lack muscular control. Anecdotally, when these factors are managed appropriately, the symptoms experienced by the patient can be reduced.
This is not to say that imaging is not required, but rather to emphasize that physical therapy should always be attempted first. There is a time and place for imaging. Trust your healthcare professional (e.g. physical therapist, sports physician, specialist etc.) before seeking further investigations.
Although there are diagnostic physical assessments, they are typically not accurate and can indicate other injuries. To help with diagnosis, an individual’s symptoms and mechanism of injury should coincide with that of a labral tear. Additional information such as aggravating movements, location of the injury, family history and daily activities will also be used to determine a diagnosis.
One test commonly used to diagnose acetabular (hip socket) injuries is the FADIR test. Although this test is considered sensitive, it is also non-specific. Meaning that if this test triggers symptoms, it indicates the presence of a hip condition but not specifically due to any labral compromise. Although this test is most accurate when performed by a healthcare professional, the video below will show how to reciprocate it individually.
Conservative treatment
Under most situations, a labral tear should be managed conservatively under the guidance of a physical therapist. This study found that 100% of patients whose condition improved, had some sort of conservative treatment. Additionally, 44% of all patients were able to avoid surgery altogether after 1-year follow-up. Although there are certain situations (e.g. high impact trauma, motor vehicle accidents etc.) where this is not an option and a specialist opinion should be sort immediately. Conservative management should involve:
- Education about the injury, prognosis and management plane
- Manual treatment techniques such as joint mobilizations and soft tissue massage
- Unloading the labrum (e.g. limiting weight-bearing activities such as jumping/running, reducing activities which require large ranges of motion)
- Specific exercises focusing on neuromuscular control and hip stability. Exercises should be continually progressed per the patient’s improvement and symptoms.
- Gait retraining
- Additional injury management strategies using electrophysiological units such as TENS/EMS machines. These devices can treat deeper structures, such as the hip joint, compared to hands-on treatment.
Below are a few general exercises that may be beneficial for the first phase of rehabilitation. However, this should not supplement the guidance of an actual physical therapist. If the exercises begin to aggravate symptoms, they should be ceased or modified accordingly with your therapist
|
Exercise |
Rationale |
Volume |
|---|---|---|
| Glut squeeze |
10-12 repetitions, 5 second holds, 3-4 sets/day |
|
| Adductor squeezes | ||
| Isometric abduction holds | ||
|
A great exercise to engage hip/back strength and core stability. Doesn’t push the hip into aggravating positions |
10-12 repetitions, 3 second holds, 3-4 sets/day |
|
|
These 2 exercises are a gentle way of strengthening the hip flexors and extensors. This avoids weight bearing on the affected leg to reduce compressive forces on the hip joint. |
10-12 repetitions, 3 second holds, 3-4 sets/day |
Table 1. Exercises recommended for the early stages of conservative treatment
Surgical Management
As mentioned, most surgical management of labral tears should be considered after 6-12 weeks of physical therapy treatment. A joint decision should be made between the specialist and physical therapist before the surgery. Each specialist may have a different recommendation on the type of surgery when considering: the type of injury/injuries, severity and individual differences.
Following the surgery, the specialist will generally recommend a list of restrictions to help recovery. Commencement of rehabilitation and physical therapy will generally occur within the first week after surgery. Below will be a general post-operative rehabilitation protocol published in the North American Journal of Sports Physical Therapy. However, it is important to discuss these specific issues with the specialist.
|
Phase |
Goal |
Management |
|---|---|---|
| Phase 1 (Week 1-4) |
|
|

